Engineering New Blood Vessels: The Future of iPSC Therapies for Cardiovascular Disease
Every year, millions of people around the world suffer from the devastating effects of peripheral artery disease (PAD) and coronary artery disease (CAD), conditions where restricted blood flow starves tissues of oxygen and function. Despite decades of medical progress, current treatments remain deeply invasive and potentially traumatic for patients. These approaches don’t address the underlying problem: the body’s inability to regenerate its own vascular network.
But what if we could reprogram the body to grow new blood vessels—precisely, safely, and with cells derived from the patient’s own tissue?
That’s the vision behind Karis Bio’s pioneering autologous iPSC-derived endothelial cell (iPSC-EC) therapy. With our newly announced collaboration, Cellino is proud to support this breakthrough by enabling industrial-grade, patient-specific cell manufacturing at scale—advancing the infrastructure needed to translate innovation into impact.
Together, we’re advancing the world’s first Nebula™-powered autologous iPSC therapy for cardiovascular disease.
Turning Back the Clock on Damaged Vasculature
Karis Bio, led by CEO and cardiologist Dr. Young-sup Yoon, is tackling cardiovascular disease with a bold and beautifully intuitive approach: rebuild the body’s natural vascular architecture using a patient’s own cells. Their strategy harnesses the promise of regenerative medicine—reprogramming somatic cells into iPSCs and guiding them into becoming endothelial cells, the same cells that line our blood vessels and drive vascular repair.
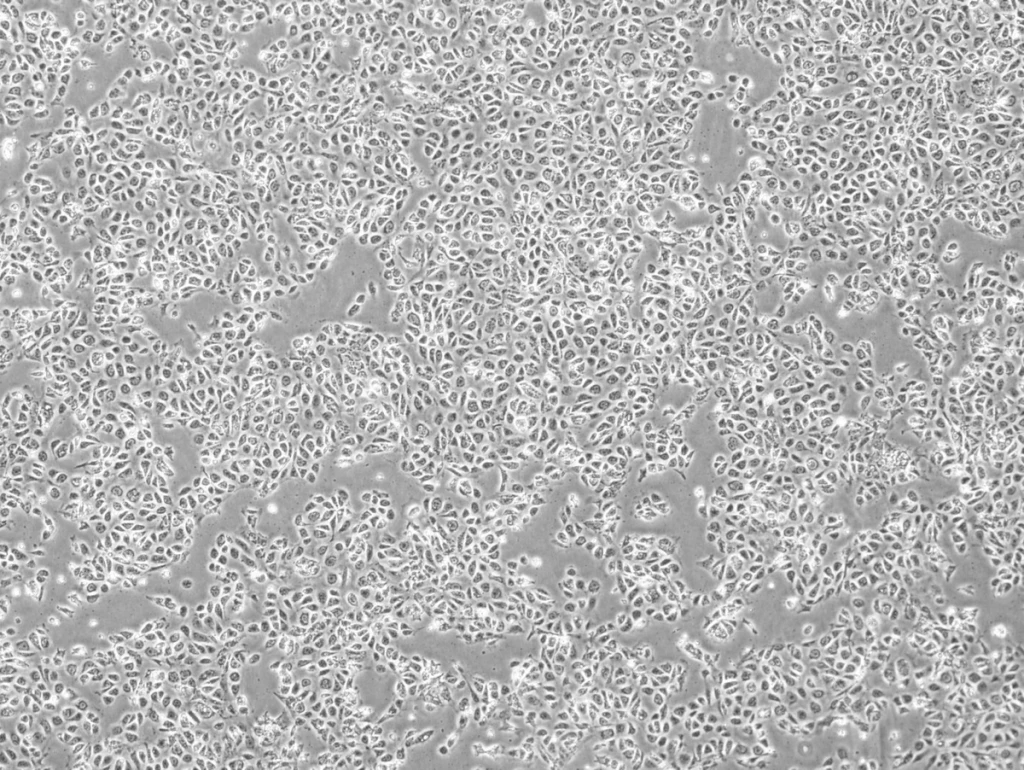
Karis Bio iPSC-Derived Endothelial Cells. Photo credit: Karis Bio
These iPSC-derived endothelial cells are then delivered back into ischemic tissues, where they trigger the formation of new blood vessels and restore circulation.
Unlike allogeneic approaches, which carry risks of immune rejection and require immunosuppressive regimens, Karis Bio’s therapy is fully autologous. That means the cells come from the patient and go back into the same patient, minimizing immunological risk while maximizing biological relevance.
The early preclinical data is promising: robust angiogenesis, improved blood flow, and functional recovery in ischemic models. Now, for the first time, this platform is moving into human testing through Karis Bio’s first-in-human clinical study, which is launching in South Korea.
Why the Manufacturing Challenge Is the Bottleneck
Despite the promise of autologous iPSC-derived therapies, clinical progress has been limited, largely due to manufacturing challenges. Producing high-quality iPSCs from individual patient samples has historically been time-consuming, expensive, and error-prone. Traditional methods rely on skilled operators carrying out high-precision manual steps in sterile cleanrooms, leading to limited scalability.
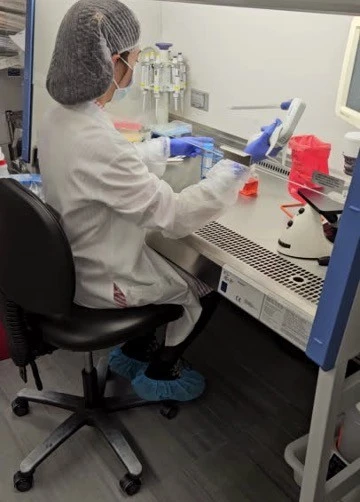
Caption: Ph.D. scientist manually culturing iPSC colonies
For autologous iPSC derived therapies to scale to the millions of patients who need them, a new manufacturing paradigm is required. That’s where Cellino comes in.
Our Nebula™ platform is designed specifically to overcome key bottlenecks in personalized cell manufacturing. Nebula™ is an autonomous, AI-driven biomanufacturing technology that automates the iPSC generation process within a compact, patient-specific cassette. With laser-based precision and machine learning, it ensures reproducibility while minimizing human error.

Caption: Cellino automated iPSC biomanufacturing workcell
Why Cardiovascular Disease Is the Perfect Test Case
While cell therapy has made headlines in oncology, cardiovascular conditions like PAD and CAD remain underserved by regenerative approaches. This is due in part to the complexity of vascular biology, but also to a lack of scalable, personalized tools to address it.
Karis Bio’s therapeutic hypothesis is bold: that by regenerating the vasculature, we can restore not just circulation, but also organ function, mobility, and quality of life. If successful, this therapy could replace the need for stents and surgeries in a subset of patients and perhaps one day, even prevent progression in high-risk populations.
South Korea’s integrated research networks and supportive regulatory environment make it a powerful setting for early clinical development. In parallel, Karis Bio’s U.S. arm—based in Atlanta—will lead future clinical studies within the U.S.’s globally recognized ecosystem for advanced therapeutic development.
Building Toward a Global Future for Autologous Therapies

This collaboration also marks Cellino’s entry into the Asia-Pacific region and reflects our shared vision with Karis Bio to make autologous regenerative therapies globally accessible.
We believe the future of biomanufacturing is decentralized: one where compact, autonomous systems like Nebula™ can be deployed in clinics and hospitals worldwide. We recently announced our collaboration with Mass General Brigham’s Gene and Cell Therapy Institute to launch the world’s first hospital-based autologous iPSC Foundry at the Massachusetts General Hospital in Boston and are excited to continue pushing the boundaries of what’s possible for patients. By removing the need for centralized cleanrooms and enabling on-site production, we can bring cell therapy closer to the patient, reduce costs, and streamline clinical logistics.
As cardiovascular disease continues to claim lives around the world, we must pursue therapies that don’t just patch damaged systems, but truly regenerate them. With the right science and the right tools, that future is finally within reach.
